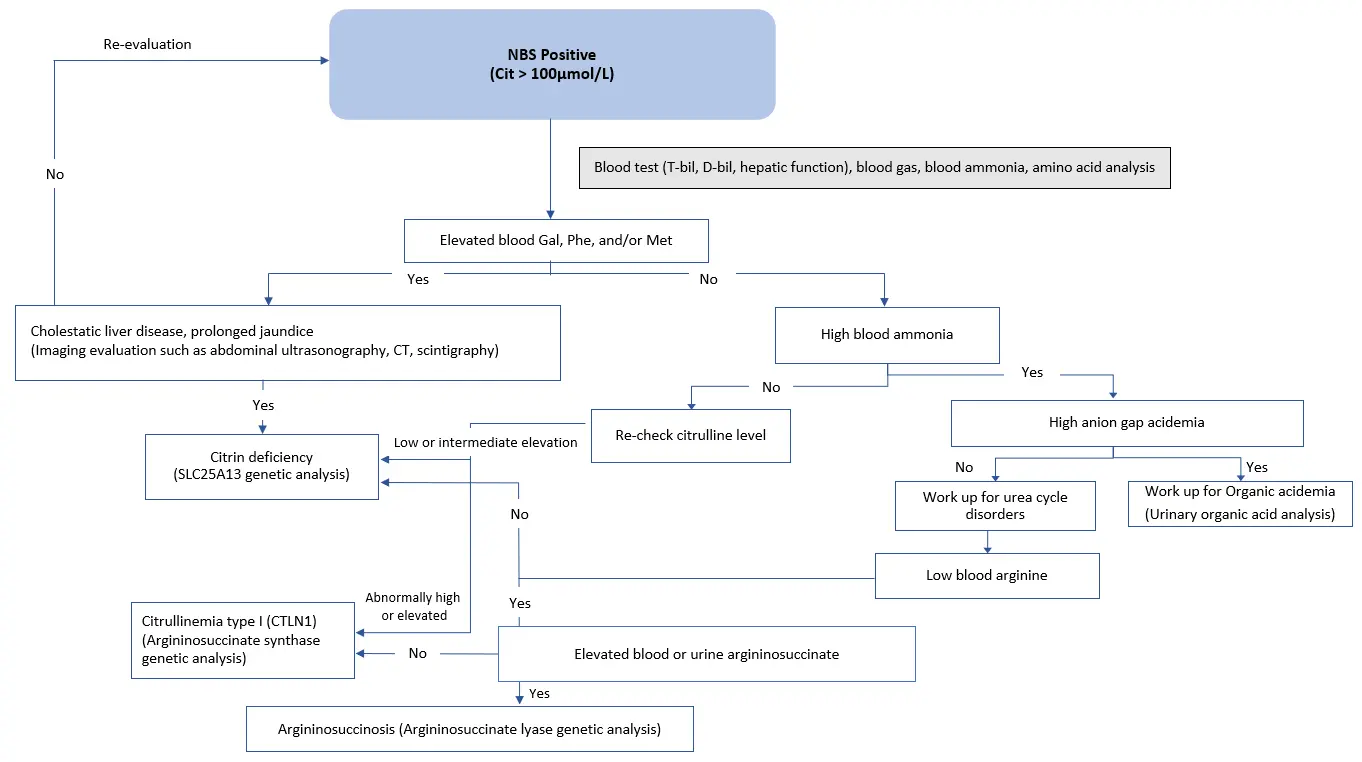
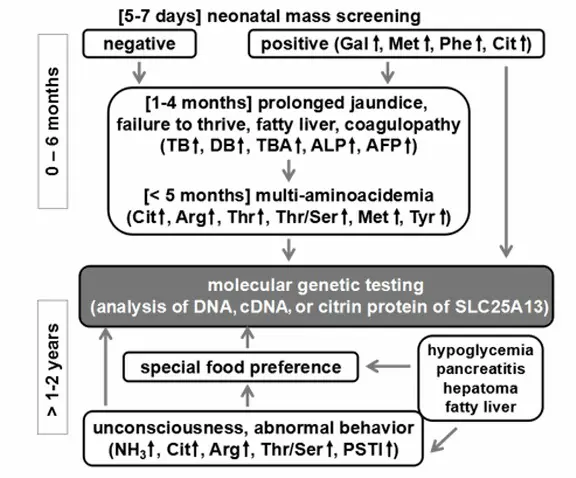
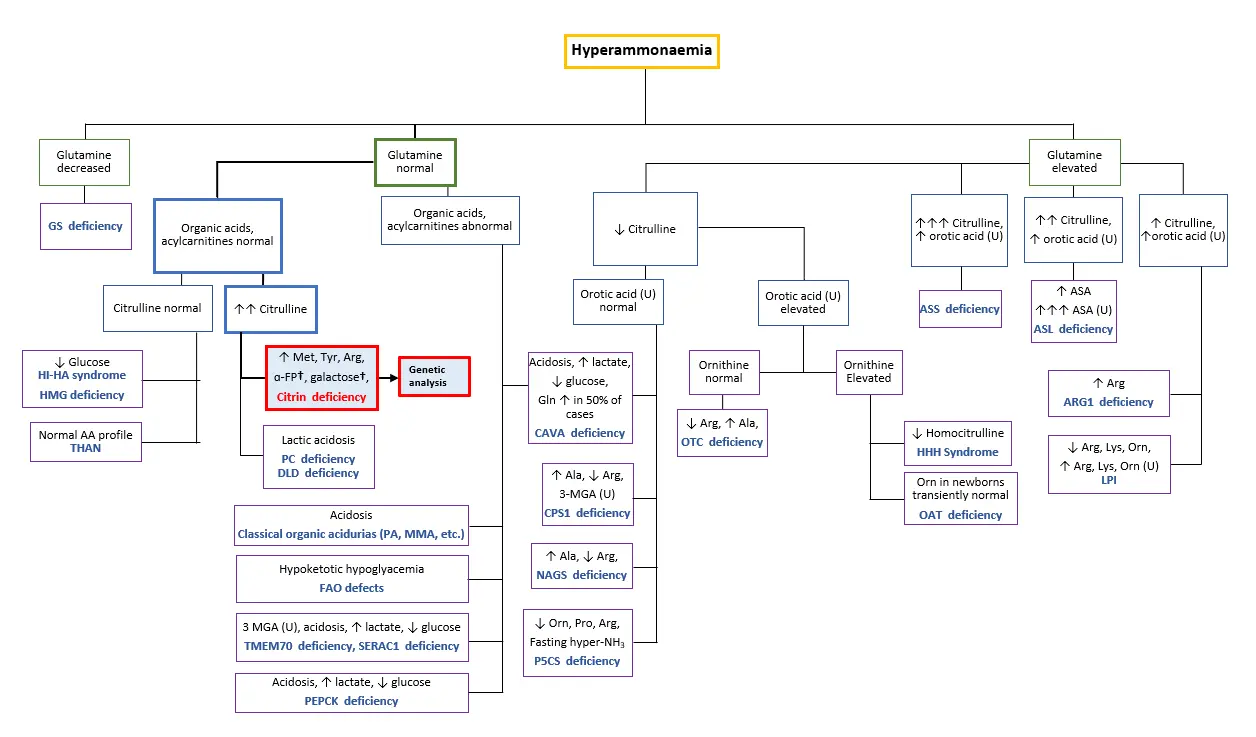
The diagnosis of citrin deficiency (CD) is based on clinical presentations and biochemical analysis (Table 1), with genetic analysis of the SLC25A13 gene being the gold standard. Patients suspected of CD should be referred to DNA testing for a confirmed diagnosis and if a genetic mutation in the gene is identified, a definite diagnosis of CD can be made. The following sections detail the specific diagnosis associated with each CD phenotype.
TABLE 1. Biochemical findings in citrin deficiency by phenotype [Adapted from Saheki & Song 2005; last updated 2017]
| Phenotype (Age) | Blood or Plasma Concentration of Ammonia (umol/L) | Plasma or Serum Concentration of Citrulline (C)# | Plasma or Serum Concentration of Arginine (A) (umol/L) | Plasma or Serum Threonine-to-Serine Ratio | Serum Concentration of Pancreatic Secretory Trypsin Inhibitor (PSTI)^ (ng/mL) |
|---|---|---|---|---|---|
| Control | 18-47* | 17-43* | 54-130* | 1.10 | 4.6-20* |
| NICCD (0-6 months) | 60 | 300 | 205 | 2.29 | 30 |
| FTTDCD | Normal or slightly elevated | Normal or slightly elevated | Typically normal | Unknown | Unknown |
| Adolescent and Adult Citrin Deficiency (AACD)* | 152 | 418 | 198 | 2.32 | 71 |
# Citrullinemia, which can be detected on newborn screening, is the earliest identifiable biochemical abnormality of NICCD [Tamamori et al 2004].
^ Because the serum PSTI concentration is high in some individuals with NICCD [Tamamori et al 2002] and also in individuals before the onset of AACD* [Tsuboi et al 2001], the measurement of serum PSTI concentration may be useful in the pre-symptomatic diagnosis of AACD*.
* Range
PHENOTYPES
*Previously known as Citrullinemia type 2 (CTLN2)
Please find the list of references here.